Most practitioners of women’s health are familiar with the terms vulvovaginal atrophy and atrophic vaginitis. Many women with this condition, also are familiar with these terms. However, they can be quite inadequate and not precise enough for describing the actual physical changes that are occurring and the symptoms that result from these changes that occur with the vulva, vagina and/or lower urinary tract that is associated with lowering of the body’s natural production of estrogen. The term vulvovaginal atrophy describes what the postmenopausal vulva looks like but doesn’t describe the associated symptoms. The term atrophic vaginitis implies inflammation or even infection, even though neither of these is the primary aspect of atrophic changes of the vulva and/or vagina.
I know that I always feel quite impolite and sound somewhat rude or at least insensitive, when I use the term vulvovaginal atrophy or atrophic vulvovaginitis with my patients. I think it imparts an excessive aging image, when these changes are in fact within the realm of normal. Neither of the current terms properly addresses the changes in the lower urinary tract. Other previous urogenital terminology changes have been useful, in both men and women… examples include overactive bladder (in place of urge incontinence, and erectile dysfunction instead of impotence).
Recognizing these issues, the board of directors of the International Society for the Study of Women’s Sexual Health (ISSWSH) and the North American Menopause Society (NAMS) cosponsored a terminology consensus conference in May of 2013. Experts in the field were selected and the relevant scientific literature was reviewed. Participants were then separated into 3 groups to determine a more descriptive, comprehensive and accurate terminology for practitioners, patients and the media. Each of the 3 groups then proposed terms to the entire consensus group for discussion and assessment. Through this process, potentially acceptable terms were voted on. The final two choices were further discussed and then a consensus was met. The process and consensus results were presented at the 2 scientific meetings of ISSWSH (February 2014) and NAMS (October 2013). The boards of both organizations then approved the new term, genitourinary syndrome of menopause (GSM).
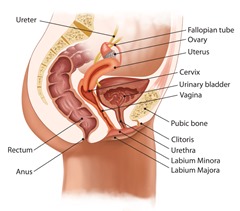 GSM is now defined as a collection of symptoms and signs associated with a decrease in estrogen and other sex steroids involving the changes to the labia majora/minora, clitoris, vestibule/introitus, vagina, urethra and bladder. These physical signs may include anatomic changes (ex/ thinning of the vulvar and/or vaginal tissue, a thin and smaller labia majora, a narrowed introitus- vaginal opening). The physiological changes result in reduced vaginal blood flow, diminished lubrication, decreased elasticity of the vaginal wall, an increased vaginal pH and decreased vaginal flora with loss of lactobacilli. The syndrome can include, but is not exclusively limited to genital symptoms of dryness, burning and irritation, fissuring of vulvar tissue, and bleeding after sex; sexual symptoms of decreased lubrication, discomfort or pain with vulvovaginal touch/penetration, and impaired arousal/orgasm functions; and urinary symptoms of urgency, dysuria and recurrent urinary tract infections. Women with GSM can present with some or even all of the signs and symptoms which must be bothersome to indicate the diagnosis and without some other diagnosis that accounts for the symptoms.
GSM is now defined as a collection of symptoms and signs associated with a decrease in estrogen and other sex steroids involving the changes to the labia majora/minora, clitoris, vestibule/introitus, vagina, urethra and bladder. These physical signs may include anatomic changes (ex/ thinning of the vulvar and/or vaginal tissue, a thin and smaller labia majora, a narrowed introitus- vaginal opening). The physiological changes result in reduced vaginal blood flow, diminished lubrication, decreased elasticity of the vaginal wall, an increased vaginal pH and decreased vaginal flora with loss of lactobacilli. The syndrome can include, but is not exclusively limited to genital symptoms of dryness, burning and irritation, fissuring of vulvar tissue, and bleeding after sex; sexual symptoms of decreased lubrication, discomfort or pain with vulvovaginal touch/penetration, and impaired arousal/orgasm functions; and urinary symptoms of urgency, dysuria and recurrent urinary tract infections. Women with GSM can present with some or even all of the signs and symptoms which must be bothersome to indicate the diagnosis and without some other diagnosis that accounts for the symptoms.
A full description of the process, new terminology and comprehensive description is found in the paper cited in the citation for this column below.
Reference
Portman D, Gass M. and consensus panel. Genitourinary syndrome of menopause: new terminology for vulvovaginal atrophy from the International Society for the Study of Women’s Sexual Health and The North American Menopause Society. : 1063-1068

